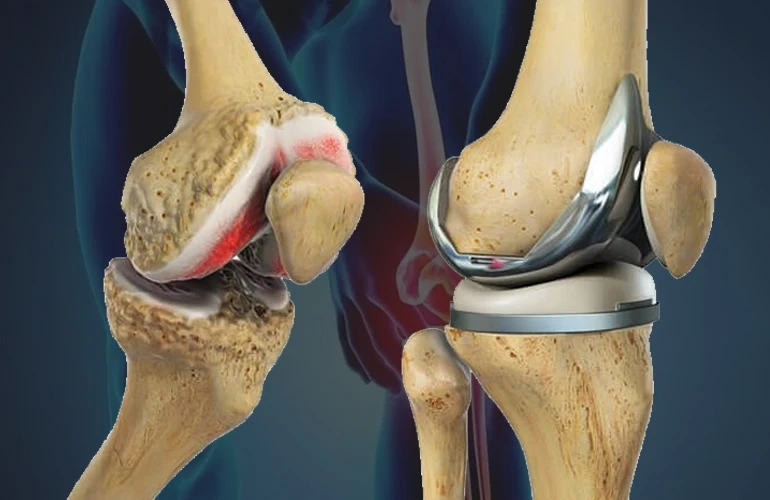
Severe knee pain is usually caused due to wear and tear of the cartilage covering the knees. Cartilage cushions the bone ends within each joint by acting as a shock absorber. Cartilage breakdown results in painful bone-on-bone contact in the knee joint. Osteoarthritis is one of the most common causes of cartilage breakdown in the knee. Genetics, age, obesity, past joint injuries like torn ligaments or fractured patella also increase the risk of osteoarthritis.
Other causes of painful knees include rheumatoid arthritis, traumatic knee injury causing permanent joint damage, childhood arthritis damaging knees during growth, osteonecrosis affecting blood supply to knee bones, weak knee ligaments leading to instability etc. Severe knee pain interfering with daily life activities and not responding to conservative treatments like medications, injections, physical therapy is usually an indication for replacement.
Different Types of Replacements
Total knee replacement (TKR) involves replacing both bone ends and cartilage surfaces. This is recommended for severely damaged knees affecting the weight bearing surfaces.
Partial knee replacement or unicompartmental knee replacement involves replacing only one of the three-compartment femoral condyle (medial or lateral) and tibial plateau. This type of surgery preserves more of the natural knee compared to TKR. It is suitable for selective cartilage damage confined to one compartment.
Revision knee replacement surgery is performed to fix or replace older worn knee implants. Knee revision is complex due to altered anatomy and bone defects. It may require implants of special design, bone grafts or realignment procedures.
Bicompartmental knee replacement falls between TKR and UKR. It involves replacing surfaces in two of the three compartments- medial and lateral femoral condyles paired with the tibial plateaux.
Procedure
Modern replacement surgery is usually performed under general or spinal anesthesia. It can be done through either midline incision or small lateral incisions. The procedure involves removing diseased bone & cartilage ends and replacing them with metal alloy and high-density plastic implants which resembles natural knee motion and alignment.
Implant components include- femoral component replacing distal femur, tibial component replacing top of tibia, sometimes patellar component replacing back of kneecap. Bone cement may be used to securely fix implants. Incisions are closed with absorbable sutures or staples. It generally takes 1-3 hours for the full procedure.
Post-operative Rehabilitation
Immediate post-op care involves pain management, wound care, leg elevation, deep breathing & ankle exercises to prevent blood clots. Patients use crutches or walker initially and later graduate to a cane or no support. Physiotherapy focusing on range of motion, strength exercises is started as early as next day to regain knee mobility.
Outpatient physical therapy continues for many weeks along with home exercise program. Returning to low impact activities like swimming, cycling begins at 4-6 weeks. Stationary or outdoor walking distances increase gradually. Light daily activities may be resumed in 4-6 weeks but heavy lifting, running, high impact sports take longer like 3-6 months or more depending on implant design and individual recovery. Repeat x-rays check for implant fixation.
Success Rates and Complications
About 90% of these surgeries are considered successful in reducing pain and improving joint function. Implant lifespan averages 15-20 years. Complications can include infection, blood clots, implant loosening or wear, stiffness, patellar complications, and ligament damage from trauma. Implant recalls due to design or manufacturing defects are rare. Overall satisfaction rates are very high among most knee replacement recipients experiencing significant pain relief and return to normal daily life activities.
Outlook and Future Directions
Advances in implant materials, designs, and computer navigation are now allowing more precise surgery, quicker recovery and better functional outcomes. Gender specific implants, patient specific implants designed based on individual joint anatomy are newer options. Bone preserving partial or resurfacing procedures could potentially expand indications for younger patients. Long term implant survival rates continue to improve with quality implants, advanced fixation techniques and minimally invasive procedures. Knee replacement surgery remains one of the most successful and commonly performed orthopaedic procedures worldwide to restore mobility and relieve pain for patients with advanced knee arthritis and other joint disorders.
Breaking Boundaries: Redefining Mobility with Knee Replacement