Reimbursements from insurance payers form the backbone of a healthcare provider’s revenue stream. After having provided medical services to a patient, the provider fills out the necessary information and sends a claim over to the payer. The payer processes it, and if everything is in order, pays the provider. But not all claims are accepted. Some are rejected even before they make it to processing, but many others are denied. Denied claims cost providers dearly and it becomes necessary to address the causes of denials.
In light of this, solutions for healthcare denial management software processes have become extremely important for small clinics with a few physicians, as well as large hospitals. Whenever a claim is denied, there is a process of appealing the denial. This again costs the providers time and money. It is important for healthcare denial management software to involve functionality that streamlines the activities in the denial management and appeals workflow.
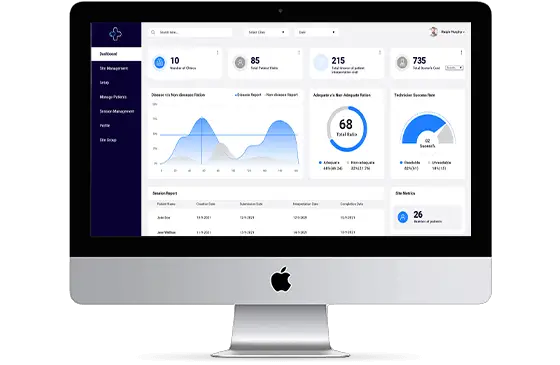
When planning to invest in a healthcare denials management software, it is important to consider the features of that solution. Let’s look at some of the important functions that a medical claims denial management platform ought to have as is the case with just about every industry, analytics solutions help assess business operations and highlight patterns that might provide insights to users. The same holds good for healthcare denial management solutions workflows. There are various reasons why a claim might get denied. It could be mistakes in filling the claims, missing codes or authorizations, or if the treatment might not be considered necessary. Whatever it might be, it helps to know why claims from a provider get denied.
This knowledge helps them implement measures to ensure that the workflow around claims is free of any errors that might get it denied. To sum it up, it helps providers learn what they were doing wrong and correct the mistakes.