It turns out that sex hurts way more often than you would
think.
In fact, pain is probably the single most common concern of women* who come to talk to me about their sex lives.
It may surprise you to know that menopause is the culprit for a lot of this pain (though there are many other causes). As is breastfeeding. As is anything else that decreases estrogen levels.
This pain can feel like burning, tearing, ripping, or stabbing with any attempt at vaginal penetration. One woman poetically described it as feeling, “like there are razor blades in there any time we try to have sex.”
That creates quite a mental image.
To make matters worse, the vulvovaginal tissue may not just be painful during sex, but can feel irritated and create mild misery all the time. Every time you wipe with toilet paper or a wash cloth. Every time you put on jeans or even underwear.
But wait there’s more! You can also feel have irritation or burning in the urethra that feels like a UTI. But there’s no infection. It’s just menopause.
Or maybe you are one of the unlucky women who will actually get more frequent UTIs when estrogen drops.
Your Vulva, Clitoris & Vagina at Puberty
Why does not having a period any more have such a profound effect on the vulva and vagina?
To answer this, let’s first think back to what happens to vulva and vagina when they were first exposed to estrogen at puberty.
If you check out a textbook of human development, you will see the Tanner Stages described. These stages outline the stereotypical development of so-called secondary sexual characteristics in boys and girls.
As sex hormones come online, girls are described as developing breasts, pubic hairs, and periods. The observers of human development noticed that boys get pubic hairs too, but surprisingly (not surprised) their genitals are also a point of interest, as much attention is paid to the growth of the testicles and penis.
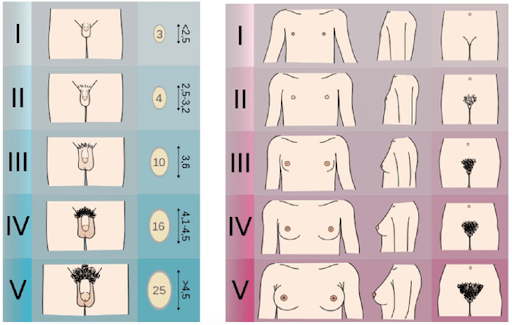
But the fine Mr. Tanner and his colleagues do not describe what happens to the vulva, clitoris and vagina at puberty. Surprised? Not surprised.
And since your textbooks and your doctors never thought about this much, you likely haven’t considered it either.
So, what does happen?
Well, it turns out that the vulva, vagina and clitoris are just as sensitive to the onset of puberty and sex steroid hormones as is the penis.
The lovely labia thicken and grow in length. The skin of the vulva may shift to darker shades of pink and brown.
The wondrous clitoris lengthens and expands, becoming more visible especially during arousal (for more on the real anatomy and physiology of the clitoris).
The marvelous vagina lengthens and becomes more flexible. The introitus or opening of the vagina widens. Secretions from the cervix and vagina increase, which helps with lubrication and fertility.
Inside the vagina, the friendly microbiome, which is essential to vaginal health, matures and stabilizes to fight off infection.
In short, the development of the vulva, vagina, and clitoris is a major event in puberty. It should be recognized and celebrated! So here is my belated congratulations!
PUBERTY IS DRIVEN BY ESTROGEN…MOSTLY
The changes that happen to the body at puberty are orchestrated by a wide array of hormones.
In general, we think of this being primarily about rising estrogen levels for vulva owners and dictated by testosterone for penis owners. When it comes to genital development, this is largely true as it is estrogen that turns on the cellular machinery that causes the vulva, clitoris and vagina to mature.
Other hormones are relevant, though. These hormones likely play a more subtle, but essential role. However, because researchers have seemed mentally wedded to the idea that “women = estrogen” and “men = testosterone,” our knowledge of this is limited.
But women make also make a slew of other hormones, including testosterone and progesterone.
We have rather recently discovered that testosterone is essential to vulvovaginal health. Testosterone is an important contributor to the vulvovaginal tissues ability to produce lubrication. In addition, the opening of the vagina (called the vestibule) can be very sensitive to testosterone levels. In fact, without enough testosterone, you may get the same kind of pain that you get without enough estrogen. Testosterone is also vital to clitoral health, helping to maintain good blood flow which supports pleasure and arousal. (https://pubmed.ncbi.nlm.nih.gov/27914563/).
So, vulvas, clitorises and vaginas love estrogen. No doubt about it. But they also wouldn’t mind a little testosterone, too.
Though I love progesterone for many things and think it is an underrated hormone for women’s health and wellness, it doesn’t seem to play an important role in vulvovaginal health.
Ok, so we have reviewed that estrogen is necessary to get the ball rolling “down there” at puberty. But the cellular machinery that is turned on at puberty doesn’t just need a one-time hit of estrogen. It needs at least a minimal amount of estrogen at all times to keep going. At that is just what they get as estrogen rises and falls with the menstrual cycle.
YOUR VULVA AND VAGINA OFF ESTROGEN
The vulva, clitoris and vagina are exposed to estrogen throughout the waxing and waning phases of the menstrual cycle. Estrogen levels rise and fall in relatively predictable patterns when you bleed or ovulate. When this cycle slows or stops, estrogen levels drop to nothing.
This can be a normal process of aging. This is what happens in menopause.
But it doesn’t just happen at menopause. Breastfeeding women can also lose their period for months to years.
It can happen to people born with vulvas but who are on estrogen blockers and testosterone as part of gender transition.
Women under extreme stress can stop having cycles. So can women who are enduring treatment for cancer or who are suffering from other illnesses.
If estrogen is essential to the development and health of the vulva, vagina and clitoris, what happens when it goes away?
What happens is that the same cellular machinery that was turned on at puberty when estrogen came on board, is now turned off. Every person will experience this differently but the underlying process is the same.
It is important that every woman understand what can happen so that if symptoms develop they know why and what can be done about it. What follows is a list of potential changes that can happen. This is not meant to make you worry but rather it is meant to empower! Here is general process that happens:
- Loss of cushion. The layer of tissue that provides cushioning under the skin
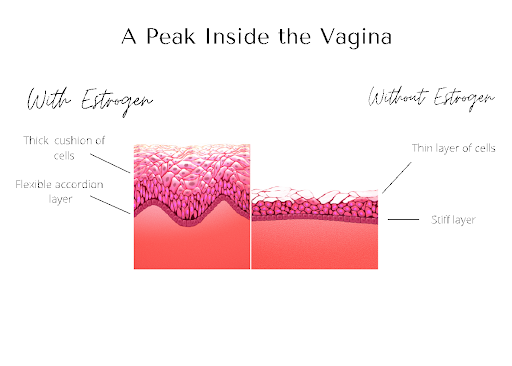 of the vulva and vagina shrinks.
of the vulva and vagina shrinks. - Loss of flexibility. Before menopause there is a layer of tissue under the skin that is pleated like…well like a pleated skirt. This allows it to stretch easily. Without estrogen, this tissue becomes flat and rigid.
- Loss of lubrication. Estrogen (and testosterone) supports the cervix and the vagina to secrete lubrication. No estrogen equals a drop in lubrication.
- Changes to the microbiome and increased pH. Estrogen helps the vagina produce glycogen – the food source for your bacterial friends in the vagina – lactobacillus. Without lactobacillus, the microbiome shifts and the pH goes up. This can change the odor of the vagina – which can be really distressing.
- Decreased strength of pelvic floor muscles. Decreased strength in these muscles contributes to urinary incontinence.
- Smaller labia. Not an earth-shattering problem for most people, but interesting nonetheless.
- Smaller introitus (opening to the vagina). No, the vagina isn’t going to close up. But even subtle changes in the opening which make it smaller and less flexible can lead to significant pain.
- Urethral changes. The urethra becomes larger and more prominent. It can also undergo other benign changes that lead to pain with urination. For some women, this combined with the changes to the vaginal microbiome can lead to increased UTIs.
- Potentially smaller, less sensitive clitoris. This is can affect arousal and orgasm, obviously. Women describe feeling like it takes a really, really long time to get to orgasm or that orgasm is kind of…meh.
These changes affect every person differently. However, studies suggest up to 87% of women will have some symptoms of low estrogen after menopause.
{https://pubmed.ncbi.nlm.nih.gov/33739315/}
This is called GENITOURINARY SYNDROME OF MENOPAUSE or GSM when it happens after the permanent loss of the menstrual cycle.
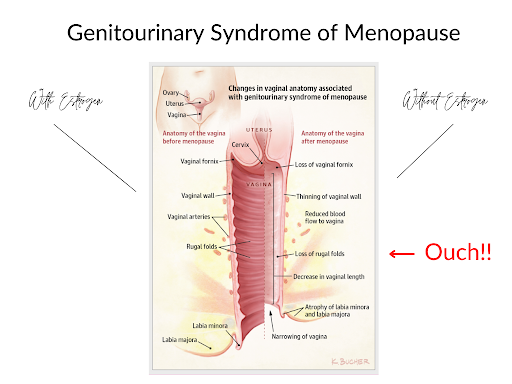
Given all of these changes, it’s pretty easy to see why sex can become so painful. Less cushion, less flexibility, less lubrication, a smaller introitus? Ouch, indeed! This is why women describe burning, ripping, tearing sensations with sex.
Again, some women may have few or no symptoms; others may find sex intolerable or have other symptoms of general irritation or urethral irritation.
But every woman should know about how estrogen affects their genitals and what can happen when it goes away. This simple information is basic to women’s ability to maintain their health and advocate for themselves as needed.
But maybe this is news to you? Or maybe you knew a little something but not all the details?
Well you are not alone.
THE PATRIARCHY STRIKES AGAIN!
How is it that a syndrome that will affect every single woman who goes through menopause and countless others is not better known?
Why is it that less than half of women have ever heard of this condition and even fewer than that have tried a tried treatment for it? { https://pubmed.ncbi.nlm.nih.gov/33739315/}
How is it that the medical establishment doesn’t provide “anticipatory guidance”? You know…could you give women a heads up about what happens and let them know what they can do about it?
Well…anybody?
Clearly, the reverberations of the patriarchy still echo throughout healthcare. The most annoying thing is that this sort of treatment of women’s issues is still so common place that we aren’t even surprised any more.
In fact, I am no longer surprised when yet another woman tells me that she has never heard of this. I am not surprised when she tells me she hasn’t had sex in several years and that she has been suffering in resigned silence.
I’m not surprised, I am just straight up angry!
From a medical standpoint, this is a very well-understood part of a woman’s life. There are clearly developed and easily accessible guidelines for how to diagnose it and how to treat it. In case you are looking for them, here they are. (https://www.menopause.org/docs/default-source/default-document-library/2020-gsm-ps.pdf)
And yet women are not taught about this and are left to suffer in silence far too often. This is quite simply totally and completely unacceptable. Women deserve better.
Women deserve information about how their body works, information about what to expect as they age or have health changes that affect their hormone levels, and accurate information about SAFE, SIMPLE, AND EFFECTIVE TREATMENTS.
Yes, that’s right. Loss of estrogen is a real problem for vulvovaginal tissue, but there are SAFE, SIMPLE, and EFFECTIVE TREATMENTS!
The medical establishment has let women down when it comes to this issue. It’s a bummer. It’s unacceptable. Though, lots of work (www.menopause.org) is being done to sensitize providers to the importance of this conversation, women are still not adequately supported.
So, let’s support each other.
I encourage you to pass this information along. It’s likely that there are people in your life who know little or nothing about this issue. Please share this with a friend, a wife, a mother, a loved one.
We can close this knowledge gap! One slightly awkward conversation about vulvovaginal health at a time! ☺
To learn more about safe treatments, check out Five Things to Know About Treating Painful Sex After Menopause.
*In this article, the term “woman” or “women” will refer to people that are born with a vulva and vagina. As we know, there are women who are not born with this genitalia and other genders who do have a vulva and vagina. Language is somewhat inept in its ability to elegantly capture this beautiful complexity. I encourage you to use the information in this article as it applies to you or your loved ones.




